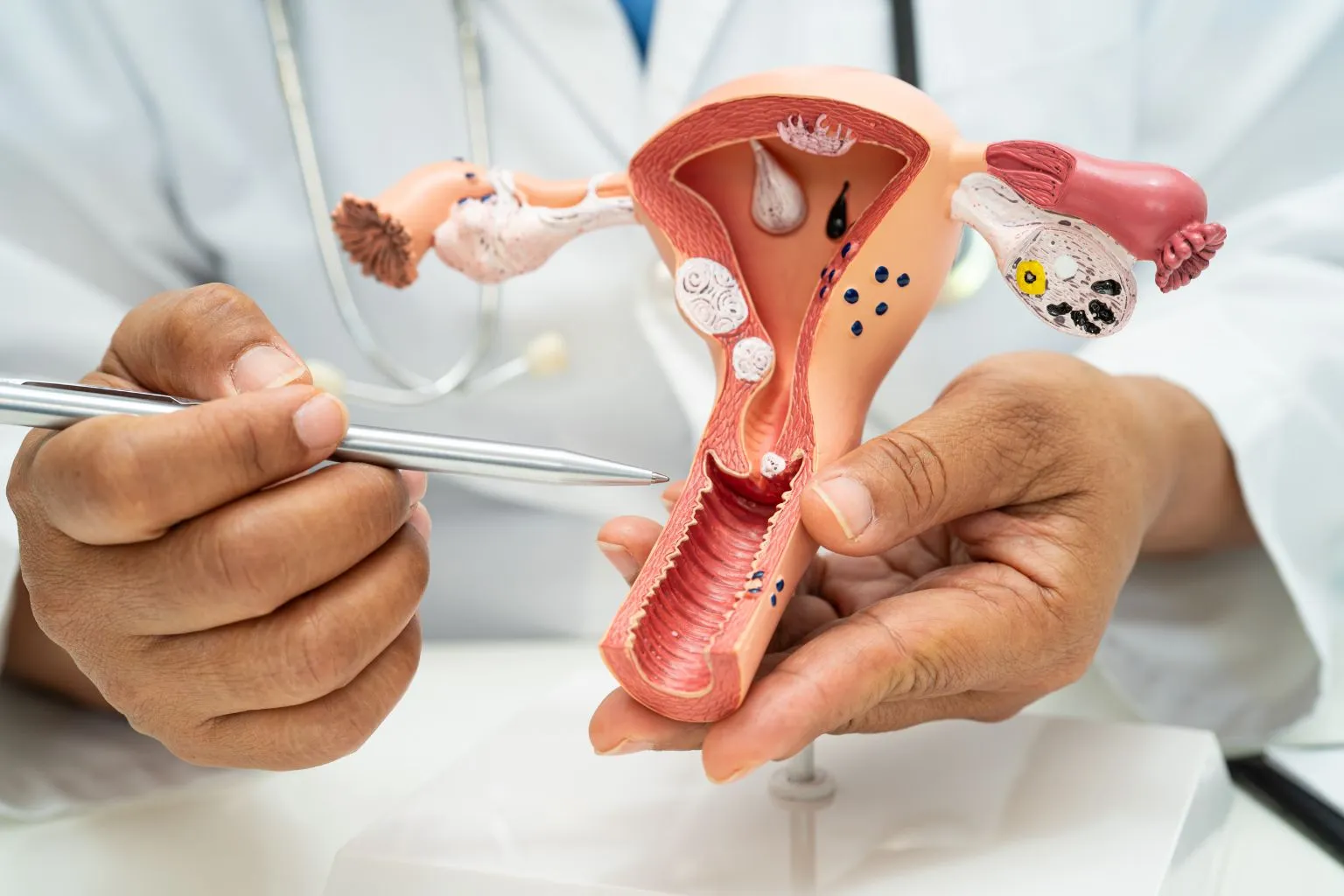
Uterine fibroids are non-cancerous growths that develop in or around the uterus, affecting many women during their reproductive years. While fibroids are usually harmless, they can sometimes cause heavy menstrual bleeding, pelvic pain, bloating, or fertility issues. When medications are not effective, surgery becomes the next step.
Two main surgical options are available – open surgery and laparoscopic surgery. Understanding the difference between these procedures is essential in deciding which one suits your case best. In this guide, Dr. Anuja Ojha from Care For Her explains everything you need to know about open surgery vs laparoscopic surgery, including their benefits, risks, and recovery times.
What Are Fibroids and When Is Surgery Needed
Fibroids are benign tumors made up of muscle and connective tissue from the uterine wall. Their size can vary from a small seed to large masses that distort the uterus. Many fibroids don’t cause symptoms, but when they do, treatment becomes necessary.
Your doctor may recommend surgical treatment if you experience:
- Heavy or prolonged menstrual bleeding
- Severe pelvic pain or pressure
- Difficulty conceiving or recurrent miscarriages
- Rapidly growing fibroids
- Fibroids are less than 10 cm in diameter
- There are fewer fibroids present
- The patient wants a faster recovery and minimal scarring
- The fibroids are located in areas easily accessible through a laparoscope
- Fibroids are very large or numerous
- Fibroids are deeply embedded in the uterine wall
- The uterus is significantly enlarged
- There are previous abdominal surgeries or scar tissues that make laparoscopy difficult
- The patient has associated complications, such as severe bleeding or pelvic adhesions
- Smaller incisions and less visible scarring
- Shorter hospital stay and faster recovery
- Reduced postoperative pain
- Quicker return to daily activities
- Lower risk of infection
- Allows removal of large or multiple fibroids
- Better visualization and control during surgery
- Suitable for complicated or high-risk cases
- Bleeding or infection
- Adhesion (scar tissue) formation
- Recurrence of fibroids over time
- Temporary fertility challenges in some cases